El Centro de la Enfermedad Inflamatoria del Intestino (EII), Gastroenterologíadentro de la División de Gastroenterología de Nicklaus Children’s Hospital, proporciona apoyo y tratamiento integrales para niños y adultos jóvenes con enfermedad de Crohn y Colitis Ulcerosa.
El objetivo es ayudar a los niños con EII para alcanzar la remisión y optimizar la calidad de vida.
Descargar libro PDF bilingue
¿Qué son las enfermedades de Crohn y la Colitis Ulcerosa?
- La enfermedad de Crohn es una enfermedad inflamatoria crónica del intestino que afecta el revestimiento del tracto digestivo desde la boca hasta el recto. La enfermedad de Crohn puede causar dolor abdominal, diarrea, pérdida de peso, anemia y fatiga.
- La colitis ulcerosa es una enfermedad inflamatoria del intestino crónica que causa inflamación en el revestimiento del intestino grueso. Los síntomas incluyen sangrado rectal, diarrea con sangre, cólicos abdominales y dolor.
El Centro de EII en Nicklaus Children’s Hospital reúne a un equipo integral de expertos para ayudar a los paciente y a sus familias en el proceso de cuidado. Todo el equipo participa en el tratamiento clínico para permitir que los niños y adultos jóvenes se beneficien de la colaboración y consulta con especialidades múltiples. Los especialistas que colaboran dentro del Centro de EII de Nicklaus Children’s Hospital incluyen nutricionistas, psicólogos/ expertos en medicina del comportamiento, expertos en el tratamiento del dolor, especialistas en terapia para niños, trabajadores sociales y cirujanos pediátricos.
Como parte de la evaluación integral, el médico puede recetarle cualquiera de las siguientes pruebas:
- Análisis de sangre de laboratorio: Estos pueden incluir análisis de sangre metabólicos integrales, vitamina D, hepatitis B, CBC (hemograma completo), PCR (proteína C reactiva), función hepática, VEB (virus de Epstein-Barr) reactivo y cuantiferón.Pruebas cutáneas: Es posible que se realice una prueba cutánea, también conocida como prueba de PPD (derivado proteico purificado), para detectar la presencia de infección por tuberculosis.
- Recolección de heces: Las pruebas de heces, incluidas una prueba funcional GI (prueba funcional gastrointestinal) y la proteína cal, son importantes en el diagnóstico y monitoreo
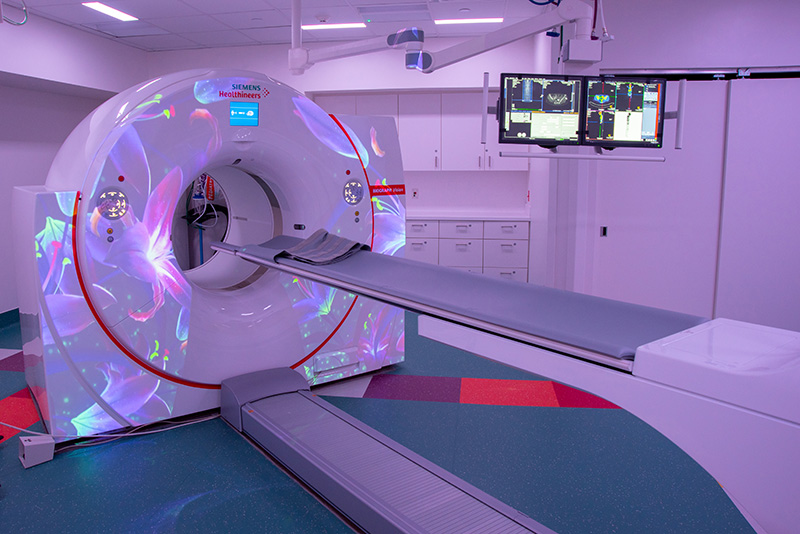
Pruebas Radiológicas
La resonancia magnética (MRI) es una prueba de diagnóstico por imágenes que produce imágenes detalladas del intestino delgado. Es posible que los pacientes no puedan comer ni beber seis horas antes de este examen. Durante este examen, el paciente deberá beber un líquido, llamado contraste oral, y se le pedirá que camine para que el contraste pueda moverse a través de los intestinos.

La CT (tomografía computarizada) es un tipo de exploración por imágenes que toma imágenes detalladas del intestino. El paciente beberá un líquido (contraste) que permite a los médicos ver el interior del intestino delgado. El paciente no podrá comer ni beber durante 6 a 8 horas antes del examen.
Los siguientes procedimientos también pueden realizarse como parte de la evaluación integral:
- EGD (esofagogastroduodenoscopia) con biopsia: Este procedimiento le proporciona al equipo de atención una vista en primer plano del tracto gastrointestinal. Se inserta un tubo flexible con una cámara en la punta a través del esófago que se usa para ver y recolectar muestras del tracto gastrointestinal.
- Colonoscopía con biopsia: Este procedimiento utiliza un tubo flexible con una cámara para tomar imágenes y muestras de los intestinos. Para prepararse para esta prueba, el médico puede recetar ablandadores de heces, enemas y supositorios. En el caso de los pacientes que no puedan beber por boca, se puede colocar una sonda nasogástrica a través de la nariz para administrar los medicamentos.
- Endoscopía por Cápsula: durante este procedimiento, una cámara inalámbrica diminuta toma imágenes a medida que pasa a través del intestino delgado. Las imágenes se registran y almacenan en un dispositivo que se usa como un cinturón alrededor de la cintura. El equipo de atención retirará el cinturón al día siguiente.
Monitoreo y Pruebas Diarias
Junto con el equipo de atención, y como parte de la evaluación integral para pacientes internados, los pacientes harán un monitoreo y seguimiento de su ingesta de alimentos, así como de las deposiciones y la orina. El equipo de atención trabajará con la familia del paciente para recopilar información como la siguiente.
- El monitoreo diario del peso se realizará antes del desayuno.
- La ingesta de alimentos y líquidos (para niños que pueden comer).
- La producción de orina y heces. El equipo de atención proporcionará a las familias un “recolector” especial que se coloca en el borde del inodoro para ayudar a recolectar muestras.
- El equipo de atención puede colocar al paciente bajo precauciones de contacto, lo que significa que es posible que el niño no pueda salir de la habitación, a menos que sea para un procedimiento, hasta que los resultados de la prueba sean negativos. Esto puede tomar entre 48 y 72 horas.
- Algunos niños tendrán una vía intravenosa (i.v.) para recibir líquidos para hidratación.
- El médico puede recetarle un descanso intestinal para darle al sistema digestivo del niño un descanso de ingerir alimentos por boca. A los pacientes en reposo intestinal se les colocará un catéter central de inserción periférica (PICC) para recibir nutrición, llamada nutrición parenteral total (TPN), y lípidos (grasas saludables). El PICC generalmente permanece en su lugar más tiempo que una vía i.v. y evita la necesidad de múltiples colocaciones i.v. A algunos pacientes se les puede colocar el PICC junto a la cama, mientras que a otros se les puede colocar anestesia en la sala de procedimientos menores.
- El médico puede solicitar muestras de sangre para hepáticas del niño. También se pueden extraer sangre para análisis de sangre de rutina del PICC.
- pacientes pueden beber batidos de reemplazo de comidas. Estos pueden tomarse por boca o a través de una sonda nasogástrica (nasogastric tube, NGT).
Dieta
Si el niño puede comer por boca, un dietista se reunirá con la familia para brindarle información sobre los tipos de alimentos que el paciente puede consumir. Las modificaciones alimenticias pueden consistir en seguir una dieta baja en fibra, baja en lactosa o sin azúcar. Las familias deben seguir las recomendaciones de los dietistas exactamente cómo se las indican, ya que son un componente fundamental para el tratamiento de la EII.
Medicamentos
El médico analizará qué medicamentos o combinaciones de medicamentos son mejores para su hijo.
- Los esteroides (metilpredinosolona) pueden administrarse por vía i.v. durante la estadía en el hospital. El equipo de atención comenzará a hacer una transición lenta del paciente de los esteroides i.v. a los esteroides orales (prednisona). En muchos casos, la terapia de dieta puede reemplazar la necesidad de esteroides.
- El médico también puede recetarle medicamentos antiinflamatorios. Vienen en forma de medicamentos orales, enemas, supositorios y espumas rectales inyectables (mesalmina).
- Durante la estadía en el hospital, algunos pacientes también pueden comenzar a recibir medicamentos inmunosupresores. Estos se pueden administrar mediante infusiones i.v. mientras que otros se administran mediante inyecciones. El médico analizará las opciones que mejor se adapten a sus necesidades.
- Según las necesidades del paciente, se puede recetar un medicamento especial para reducir la inflamación y calmar el sistema inmunitario, llamado metotrexato.
- Este medicamento se puede recibir por vía oral o como inyección.
Supplementos
El médico analizará los suplementos para ayudar con las necesidades individuales de su hijo. Estos pueden incluir vitamina D, hierro, magnesio y ácido fólico.
Atención de Seguimiento
- A los pacientes se les realizarán análisis de sangre de rutina hasta que los niveles sanguíneos del medicamento estén dentro del rango terapéutico.
- Se les pedirá a los niños que se realicen análisis de sangre anualmente para controlar sus niveles de vitaminas y otros factores importantes, incluido el cuantiferón.
- También se indicarán recolecciones de heces y procedimientos para monitorear el tubo digestivo y el colon, según sea necesario.
- Los pacientes serán derivados a un dietista clínico para ayudar al niño con sus necesidades alimentarias.
- El gastroenterólogo le indicará estudios de diagnóstico por imágenes de rutina mediante resonancia magnética (MRI) o tomografía computarizada (CT).
- También se indicarán procedimientos de rutina, como EGD o la esofagogastroduodenoscopia (EGD) ocolonoscopía. and/or colonoscopies, may also be be prescribed.
Recursos Comunitarios
Comuníquese con un miembro del equipo de atención
Para comunicarse con un miembro del Centro de Enfermedad Inflamatoria del Intenstino o para programar una cita, llame al 786-624-2546.