Authors: Redmond Burke, MD, Cardiovascular Surgery Chief and Anthony Rossi, MD, Chief, Cardiovascular Medicine.
Introduction:
The
Heart Institute at Nicklaus Children’s Hospital remains dedicated to providing the very best and safest experience for patients undergoing congenital heart surgery. Today we report 18 years of outcomes for patients undergoing the arterial switch operation for complete transposition of the great arteries who were operated by Dr. Redmond Burke.
Methods:
We reviewed our CardioAccess database for patients undergoing the arterial switch operation from January 2001 through February 2019. These dates coincide with our Real-Time Outcomes Report. The data was then filtered to include only patients who were operated on by Dr. Burke.
Operative digital imaging of each patient’s procedure was routinely used to document the anatomy and repair of each lesion. Every operation was videotaped with a camera at the head of the operating table, the video was visible to the entire team during the procedure, and was digitally stored for on demand performance review. Technical pearls include, complete mobilization of the pulmonary arteries to the hilum, native pericardium for patches, high transection of the aorta to keep the PA’s above the coronary buttons after the RVOT is reconstructed, 8-0 prolene for coronary buttons, trap doors for coronary transfer, division of single coronaries into two separate buttons, VSD repair via the RA with pericardium and running 8-0 prolene. Routine left atrial pressure monitoring is used when separating from bypass. No routine pacing wires were used.
Results:
There were 157 babies who underwent the arterial switch operation by Dr. Burke during this time period. The median weight at the time of surgery for these babies was 3.3 kgs (range 1.7-5.4 kg). They were operated on at a median age of 6 days. There were no deaths. The median postoperative stay was 9 days. There were 96 patients classified as TGA/IVS, 54 TGA/VSD (6 with muscular VSDs), and 7 as DORV. There were 7 patients who required distal aortic arch repairs for either discrete coarctation or hypoplasia of the aortic arch.
ardiopulmonary bypass times averaged 206 minutes. There were 4 patients who required a period of deep hypothermic circulatory arrest to complete their repair.
All patients were discharged home in good condition.
| Category |
Number of Patients |
Median Age |
Number of Mortalities |
NCH % Mortality |
STS1 |
| ASO and ASO/VSD |
157 |
6 days |
0 |
0% |
3.4% |
Discussion:
Jatene described the anatomic repair of complete transposition of the great arteries oin19751. This report describes a remarkable series of patients undergoing the ASO by a single surgeon in a single center. The current series compares favorably with the very best outcomes reported to date. The most recent review of patients undergoing the ASO according to the STS revealed a mortality rate of 3.4%2. Our postoperative length of stay is 40-50% less than patients undergoing the ASO or ASO/VSD according to the latest STS outcomes report3. Babies as small as 1.7 kilograms underwent a successful operation and our series included 30 patients less than 3 kilograms and 11 babies who were 2.5 kilograms or less.
There were 4 patients who had a period of deep hypothermic circulatory arrest (DHCA) during the intraoperative period (2.5%), none since 2011. The avoidance of DHCA if possible is an institutional policy, since we are not certain that any degree of DHCA can be performed safely and without neurological injury. We have found that most operations today can be performed without DHCA.
While this report highlights the remarkable skill set of a single surgeon, it is clear that surgical experience and institutional experience both play a role in best outcomes for patients undergoing the ASO. As reported by Karamlou, surgeons performing 6 ASO or more operations per year were statistically more likely to have better outcomes than those who performed less. According this this review of the STS database, the median surgical volume for the ASO was 2 per surgeon and 4 per institution. Our surgeon and program compare very favorably and surpasses these standards. While in the review by Karamlou the individual surgical experience was slightly more important than the institutional experience, programmatic experience did matter. This Nicklaus Children’s Hospital experience reflects perhaps the largest number of patients undergoing the ASO operation in the state of Florida over that time period.
Our programmatic approach to the neonate with complete transposition (D-TGA) who is admitted to the CICU is determined somewhat by the clinical condition of the baby. Generally, we see no reason for most babies to have their surgeries delayed beyond the first week of life and aim to perform the arterial switch operation within the first few days. Most babies arrive to our unit on an infusion of prostaglandin E1. We often continue this, but at the lowest dose required to maintain ductal patency. This can usually be accomplished at a dose of 0.01 mcg/kg/min for most patients. A balloon septostomy is performed only on babies who exhibit profound cyanosis, it is rarely performed on babies with a PaO2 > 35 mm Hg. Most babies will not require preoperative intubation and if breathing comfortably, we allow the baby to feed orally prior to surgery.
Components of a comprehensive cardiac surgical program that we believe help contribute to these superior outcomes include a dedicated cardiac anesthesia team, meticulous preoperative and postoperative diagnostic imaging, a dedicated CICU program and physician extenders who accumulate years of bedside experience and provide great consistency in patient care. As previously reported, point-of-care testing, serial lactate monitoring and goal-directed therapy have been shown to diminish mortality3. The development of a Real Time Outcomes Reporting tool allowed for the implementation of real time performance assessment and improvement.
Take Home Message:
The arterial switch operation can be performed successfully at Nicklaus Children’s Hospital with survival rates that surpass most contemporary reports. This is true for patients with complex TGA and for patients at low birth weights.
Images
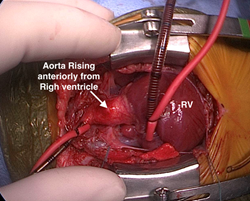 Surgeon’s view of D-TGA. Image courtesy Dr. Redmond Burke.
Surgeon’s view of D-TGA. Image courtesy Dr. Redmond Burke.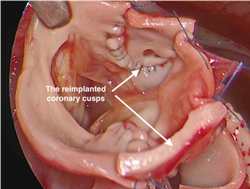 The coronary cusps are reimplanted into the neoaorta. Image Courtesy Dr. Redmond Burke.
The coronary cusps are reimplanted into the neoaorta. Image Courtesy Dr. Redmond Burke.
Videos
In this video, Dr. Burke will take you through the arterial switch operation, conducted by him.
In this video is Dr. Burke performs the ASO/VSD on a preterm infant with a single coronary artery.
Outcomes for cardiac surgical patients at Nicklaus Children’s Hospital continued to be reported in real-time and have been so since 2001. Nicklaus Children’s Hospital’s Real-Time Outcomes is the most comprehensive and transparent outcomes reporting website available today, with over 18 years of outcomes available for review.
References:
- Jatene AD, Fontes VF, Paulista PP, et al: Successful anatomic correction of transposition of the great vessels: a preliminary report. Arq Bras Cardiol 28:461, 1975.
- Karamlou T, Jacobs ML, Pasquali S, He X, Hill K, O'brien S, McMullan DM, Jacobs JP. Surgeon and center volume influence on outcomes after arterial switch operation: analysis of the STS Congenital Heart Surgery Database. The Annals of thoracic surgery. 2014 Sep 1;98(3):904-11.
- http://www.pediatricheartsurgery.com/realtimeoutcomes/cvperformance.aspx
- Rossi AF, Khan DM, Hannan R, Bolivar J, Zaidenweber M, Burke R. Goal-directed medical therapy and point-of-care testing improve outcomes after congenital heart surgery. Intensive care medicine. 2005 Jan 1;31(1):98-104.
Additional References of Interest:
- Villafañe J, Lantin-Hermoso MR, Bhatt AB, Tweddell JS, Geva T, Nathan M, Elliott MJ, Vetter VL, Paridon SM, Kochilas L, Jenkins KJ. D-transposition of the great arteries: the current era of the arterial switch operation. Journal of the American College of Cardiology. 2014 Aug 5;64(5):498-511.
- Fricke TA, d'Udekem Y, Richardson M, Thuys C, Dronavalli M, Ramsay JM, Wheaton G, Grigg LE, Brizard CP, Konstantinov IE. Outcomes of the arterial switch operation for transposition of the great arteries: 25 years of experience. The Annals of thoracic surgery. 2012 Jul 1;94(1):139-45.
- Wernovsky G, Wypij D, Jonas RA, Mayer Jr JE, Hanley FL, Hickey PR, Walsh AZ, Chang AC, Castañeda AR, Newburger JW, Wessel DL. Postoperative course and hemodynamic profile after the arterial switch operation in neonates and infants: a comparison of low-flow cardiopulmonary bypass and circulatory arrest. Circulation. 1995 Oct 15;92(8):2226-35.
- Iliopoulos I, Burke R, Hannan R, Bolivar J, Cooper DS, Zafar F, Rossi A. Preoperative intubation and lack of enteral nutrition are associated with prolonged stay after arterial switch operation. Pediatric cardiology. 2016 Aug 1;37(6):1078-84.