What is an ear infection?
Also known as: otitis media, OM.
An ear infection is an inflammation of the middle ear (the air-filled space behind the eardrum that contains the little bones that transmit the sound vibrations from the eardrum). It’s usually caused by a bacterial or viral infection, and frequently follows a cold or other respiratory infection. Children may have a number of infections each year.
Sometimes the fluid from the inflammation accumulates in the middle ear (otitis media with effusion, OME).
While anyone can get an ear infection, children get them more often than adults. Five out of six children will have at least one ear infection by their third birthday. In fact, ear infections are the most common reasons parents bring their children to their Pediatrician. Chronic otitais media, can occur without effusion or with effusion (COME) - when children have recurrent episodes of OM or when the middle ear fluid remains in the middle ear for a long time.
How can I tell if my child has an ear infection? What are the symptoms of an ear infection?
Ear infections are frequently painful. Many ear infections however happen to children before they’ve learned how to talk. If your child isn’t old enough to say “My ear hurts,” here are a few things to look for:
- Tugging or pulling at the ear(s)
- Fussiness and crying
- Trouble sleeping
- Fever (especially in infants and younger children)
- Fluid draining from the ear
- Clumsiness or problems with balance
- Trouble hearing or responding to quiet sounds
Parts of the ear
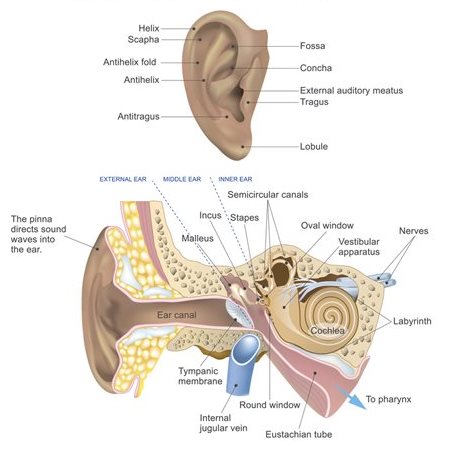
The ear has three major parts: the outer ear, the middle ear, and the inner ear. The outer ear, also called the pinna, includes everything we see on the outside—the curved flap of the ear leading down to the earlobe—but it also includes the ear canal, which begins at the opening to the ear and extends to the eardrum. The eardrum is a membrane that separates the outer ear from the middle ear.
The middle ear—which is where ear infections frequently occur—is located between the eardrum and the inner ear. Within the middle ear are three tiny bones called the malleus, incus, and stapes that transmit sound vibrations from the eardrum to the inner ear. The bones of the middle ear are surrounded by air.
The inner ear contains the labyrinth, which help us keep our balance. The cochlea, a part of the labyrinth, is a snail-shaped organ that converts sound vibrations from the middle ear into electrical signals. The auditory nerve carries these signals from the cochlea to the brain.
Other nearby parts of the ear also can be involved in ear infections. The eustachian tube is a small passageway that connects the upper part of the throat to the middle ear. Its job is to supply fresh air to the middle ear, drain fluid, and keep air pressure at a steady level between the nose and the ear.
Adenoids are small pads of tissue located behind the back of the nose, above the throat, and near the eustachian tubes. Adenoids are mostly made up of immune system cells. They fight off infection by trapping bacteria that enter through the mouth.
Why are children more likely than adults to get ear infections?
There are several reasons why children are more likely than adults to get ear infections.
Eustachian tubes are smaller and more level in children than they are in adults. This makes it difficult for fluid to drain out of the ear, even under normal conditions. If the eustachian tubes are swollen or blocked with mucus due to a cold or other respiratory illness, fluid may not be able to drain.
A child’s immune system isn’t as effective as an adult’s because it’s still developing. This makes it harder for children to fight infections.
As part of the immune system, the adenoids respond to bacteria passing through the nose and mouth. Sometimes bacteria get trapped in the adenoids, causing a chronic infection that can then pass on to the eustachian tubes and the middle ear.
How does a doctor diagnose a middle ear infection?
The first thing a doctor will do is ask you about your child’s health. Has your child had a head cold or sore throat recently? Is he having trouble sleeping? Is she pulling at her ears? If an ear infection seems likely, the simplest way for a doctor to tell is to use a lighted instrument, called an otoscope, to look at the eardrum. A red, bulging eardrum indicates an infection.
A doctor also may use a pneumatic otoscope, which blows a puff of air into the ear canal, to check for fluid behind the eardrum. A normal eardrum will move back and forth more easily than an eardrum with fluid behind it.
How is an acute middle ear infection treated?
Many doctors may prescribe an antibiotic, such as amoxicillin, to be taken over 10 days. Your doctor also may recommend over-the-counter pain relievers such as acetaminophen or ibuprofen, or eardrops, to help with fever and pain. (Because aspirin is considered a major preventable risk factor for Reye’s syndrome, a child who has a fever or other flu-like symptoms should not be given aspirin unless instructed to by your doctor.)

If your doctor isn’t able to make a definite diagnosis of OM and your child doesn’t have severe ear pain or a fever, your doctor might ask you to wait a day or two to see if the earache goes away. The American Academy of Pediatrics issued guidelines in 2013 that encourage doctors to observe and closely follow these children with ear infections that can’t be definitively diagnosed, especially those between the ages of 6 months to 2 years. If there’s no improvement within 48 to 72 hours from when symptoms began, the guidelines recommend doctors start antibiotic therapy.
Sometimes ear pain isn’t caused by infection, and some ear infections may get better without antibiotics. Using antibiotics cautiously and with good reason helps prevent the development of bacteria that become resistant to antibiotics.
If your doctor prescribes an antibiotic, it’s important to make sure your child takes it exactly as prescribed and for the full amount of time. Even though your child may seem better in a few days, the infection still hasn’t completely cleared from the ear. Stopping the medicine too soon could allow the infection to come back. It’s also important to return for your child’s follow-up visit, so that the doctor can check if the infection is gone.
How long will it take my child to get better?
Your child should start feeling better within a few days after visiting the doctor. If it’s been several days and your child still seems sick, call your doctor. Your child might need a different antibiotic. Once the infection clears, fluid may still remain in the middle ear but usually disappears within three to six weeks.
What happens if my child keeps getting ear infections?
To keep a middle ear infection from coming back, it helps to limit some of the factors that might put your child at risk, such as not being around people who smoke and not going to bed with a bottle. In spite of these precautions, some children may continue to have middle ear infections, sometimes as many as five or six a year.
Your doctor may want to wait for several months to see if things get better on their own but, if the infections keep coming back and antibiotics aren’t helping, many doctors will recommend a surgical procedure that places a small ventilation tube in the eardrum to improve air flow and prevent fluid backup in the middle ear. The most commonly used tubes stay in place for six to nine months and require follow-up visits until they fall out.
If placement of the tubes still doesn’t prevent infections, a doctor may consider removing the adenoids to prevent infection from spreading to the eustachian tubes.
Reviewed by: Richmond Darko, MD
This page was last updated on: 1/29/2019 3:21:13 PM
© 2025 Nicklaus Children's Hospital. All Rights Reserved.